| |
| |
|
Patient Information |
| |
|
Healthcare Professionals Information |
|
| |
|
| |
|
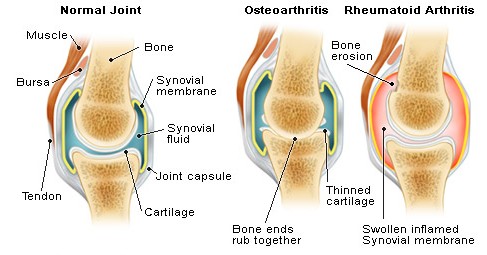
Osteoarthritis
Osteoarthritis (OS-tee-oh-arth-RY-tis) is a condition that affects the bones and joints in the body. When the cartilage that covers the ends of bones wears down, bone can rub against bone. People with osteoarthritis often feel pain and stiffness in the joints upon rising in the morning, but feel better after moving around. Osteoarthritis that is not treated can lead to disability. |
Osteoarthritis is also known as degenerative arthritis. Among the over 100 different types of arthritis conditions, osteoarthritis is the most common, affecting over 20 million people in the United States. Osteoarthritis occurs more frequently as we age. Before age 45, osteoarthritis occurs more frequently in males. After age 55 years, it occurs more frequently in females. In the United States, all races appear equally affected. |
What causes osteoarthritis?
Primary osteoarthritis is mostly related to aging. With aging, the water content of the cartilage increases, and the protein makeup of cartilage degenerates. Eventually, cartilage begins to degenerate by flaking or forming tiny crevasses. In advanced cases, there is a total loss of cartilage cushion between the bones of the joints. Repetitive use of the worn joints over the years can irritate and inflame the cartilage, causing joint pain and swelling. Loss of the cartilage cushion causes friction between the bones, leading to pain and limitation of joint mobility. Inflammation of the cartilage can also stimulate new bone outgrowths (spurs, also referred to as osteophytes) to form around the joints. Osteoarthritis occasionally can develop in multiple members of the same family, implying a hereditary (genetic) basis for this condition.
Secondary osteoarthritis is caused by another disease or condition. Conditions that can lead to secondary osteoarthritis include obesity, repeated trauma or surgery to the joint structures, abnormal joints at birth (congenital abnormalities), gout, diabetes, and other hormone disorders. Obesity causes osteoarthritis by increasing the mechanical stress on the cartilage. In fact, next to aging, obesity is the most powerful risk factor for osteoarthritis of the knees.
The early development of osteoarthritis of the knees among weight lifters is believed to be in part due to their high body weight. Repeated trauma to joint tissues (ligaments, bones, and cartilage) is believed to lead to early osteoarthritis of the knees in soccer players. Interestingly, recent studies have not found an increased risk of osteoarthritis in long-distance runners. Crystal deposits in the cartilage can cause cartilage degeneration and osteoarthritis.
Uric acid crystals cause arthritis in gout, while calcium pyrophosphate crystals cause arthritis in pseudo gout. Some people are born with abnormally formed joints (congenital abnormalities) that are vulnerable to mechanical wear, causing early degeneration and loss of joint cartilage.
Osteoarthritis of the hip joints is commonly related to structural abnormalities of these joints that had been present since birth. Hormone disturbances, such as diabetes and growth hormone disorders, are also associated with early cartilage wear and secondary osteoarthritis.
|
What is the treatment for osteoarthritis?
Aside from weight reduction and avoiding activities that exert excessive stress on the joint cartilage, there is no specific treatment to halt cartilage degeneration or to repair damaged cartilage in osteoarthritis. The goal of treatment in osteoarthritis is to reduce joint pain and inflammation while improving and maintaining joint function. Some patients with osteoarthritis have minimal or no pain and may not need treatment.
Others may benefit from conservative measures such as rest, exercise, diet control with weight reduction, physical and occupational therapy, and mechanical support devices. These measures are particularly important when large, weight-bearing joints are involved, such as the hips or knees. In fact, even modest weight reduction can help to decrease symptoms of osteoarthritis of the large joints, such as the knees and hips. Medications are used to complement the physical measures described above. Medication may be used topically, taken orally, or injected into the joints to decrease joint inflammation and pain. When conservative measures fail to control pain and improve joint function, surgery can be considered.
Resting sore joints decreases stress on the joints and relieves pain and swelling. Patients are asked to simply decrease the intensity and/or frequency of the activities that consistently cause joint pain.
Exercise usually does not aggravate osteoarthritis when performed at levels that do not cause joint pain. Exercise is helpful in osteoarthritis in several ways. First, it strengthens the muscular support around the joints. It also prevents the joints from "freezing up" and improves and maintains joint mobility. Finally, it helps with weight reduction and promotes endurance. Applying local heat before and cold packs after exercise can help relieve pain and inflammation. Swimming is particularly well suited for patients with osteoarthritis because it allows patients to exercise with minimal impact stress to the joints. Other popular exercises include walking, stationary cycling, and light weight training.
Many studies, but not all, have suggested that alternative treatment with the food supplements glucosamine and chondroitin can relieve symptoms of pain and stiffness for some people with osteoarthritis.
Learn how Flexost can help. |
|
